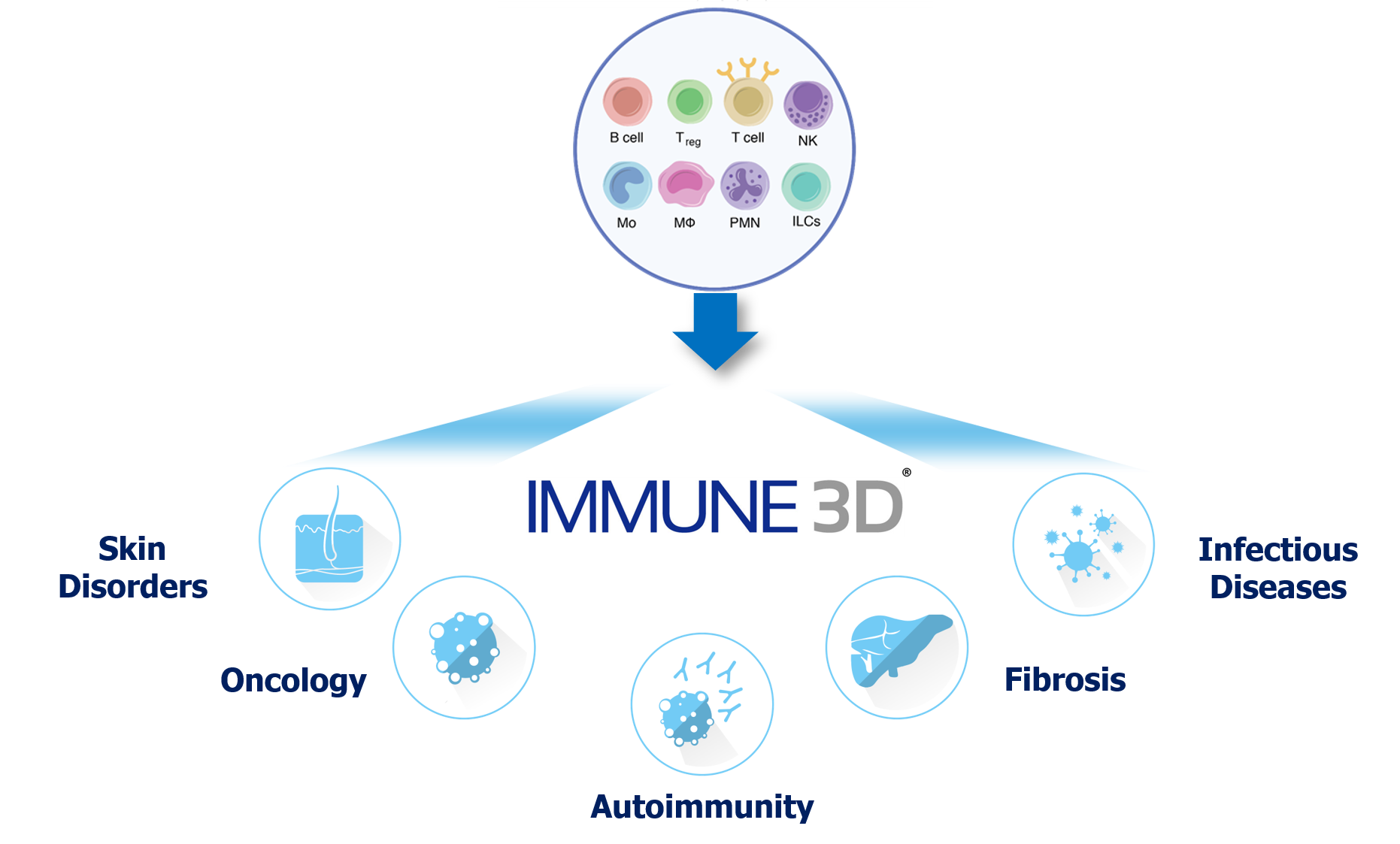
The immune system plays a role in many major diseases by protecting us against infectious agents and malignant cells or by causing disease in the case of autoimmunity. To build physiologically relevant 3D platforms begins with an in-depth understanding of disease pathogenesis and the factors that contribute to disease biology. This understanding coupled with technological advancements in data capture and real world evidence enables us to develop meaningful 3D platforms.
The skin is an essential organ to the human body and it serves as the first line of defense against major pathogens and physical and chemical insults. The skin provides a sophisticated network of effector cells, microbes and molecular mechanisms to constitute a unique system of immune surveillance. An inadequate immune response leads to infections or tumors while an excessive immune responses may lead to autoimmunity or inflammation.
Billions of microbes including bacteria and fungi that live in harmony on our skin. Despite their close proximity with immune cells including DCs (Langerhans cells) and lymphocytes that reside within the skin tissue, in general no activation of the immune system occurs. This is likely due to cross-talk between skin resident immune cells that actively avert recognition of these microbes in exchange for the benefits they provide (i.e. competition for space/nutrients with pathogenic microbes).
Therefore, studying the mechanisms that regulate or disrupt skin immune cell interactions, migration and infiltration requires sophisticated yet cost-effective systems to advance new therapeutics, cosmetics and diagnostic modalities.
IMMUNE 3D® develops systems that capture the skin environment to study factors such as:
- Role of immune cell migration such as Tregs
- Skin gamma-delta (γδ) and its role in oncology and other diseases
- Innate Lymphoid Cells (ILCs) and microbial interactions
- The evolution of the immune response to aged matrix
The clinical success in immunotherapy has paved the way for next generation of cancer drugs. However, while patients of various tumor types have experienced a favorable clinical response, a number of patients have experienced low clinical responses or present resistance to these therapies.
Advancements in technology have enabled our understanding of the causes of resistance and the role of the Tumor Microenvironment (TME). While cancer therapy primarily focuses on direct targeting of malignant cells or enhancing immune cells with tumor-specificity there are many other non-cancerous stromal cells that are a major component of the tumor microenvironment. These include fibroblasts, endothelial cells, specialized mesenchymal cells in addition to resident immune cells.
IMMUNE 3D® aims to capture the key TME cell components and environments to mimic these classifications. We leverage the use of HLA-matched Cytotoxic T Lymphocyte (CTL) and tumor cell lines and patient-derived cells across broad tumors to study the following factor:
Our focus on autoimmunity centers around diseases that remain a challenge for millions of patients and for which we can develop robust systems to effectively capture the true environments that can lead to better therapies and biomarkers for patient stratification and response.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is an chronic autoinflammatory disorder associated with joint pain stemming from immune attack of synovial membranes. While ultimately associated with debilitating joint pain, patients with RA can also have systemic involvement resulting in skin, pulmonary and cardiovascular complications. Although RA likely develops overtime through a multitude of factors, the expansion of self-antigen specific T cells and B cells that produce autoantibodies targeting synovial proteins are ultimately important in sustaining disease chronicity over time.
To this end, IMMUNE 3D® recapitulates the normal tissue components and structure will be important for understanding how targeting tissue infiltration and residence of lymphocytes will influence disease progression.
Scleroderma
Scleroderma (or systemic sclerosis) is an autoimmune disorder characterized by fibrosis (overactive collagen deposition) both in the skin and other systemic organs including the heart, lung, esophagus and kidneys. Immune cells such as macrophages (M2 macrophages), Th1 and Th17 cells are recruited during inflammation whereas the Th2 cells have been shown to be involved in disease pathogenesis. For scleroderma patients, the majority of therapeutic success involves treating patients with B cell and T cell depleting antibodies or through autologous hematopoietic stem cell transplantation (following non-myeloablation of immune cells).
IMMUNE 3D® provides an effective platform to study the role of immune cells such as Tregs and other immunosuppressive populations that could serve as potential targets for novel therapies or biomarkers of disease.
Psoriasis
Psoriasis is a chronic disease that afflicts 2-3% of the world’s population. The most common form, plaque psoriasis, is characterized by hyperproliferative skin cells (keratinocytes) that result in thick, scaly patches of skin known as plaques. More recent studies have demonstrated T cells are the predominant leukocytes within psoriatic lesions and the main driver of inflammation. To this end, treatment with broad immunosuppressants (e.g. cyclosporine) or drugs targeting T cell activation (e.g. CTLA-4 Ig) have proven effective [albeit non-specific] therapies. A pathogenic role for IL-17 producing T cells (Th17 cell) has led to development of new therapeutic strategies that directly target their effector cytokines (IL-17A) or the cytokine IL-23 that promotes the recruitment and development of Th17 cells in diseased tissue. These therapies have led to remarkable remission of symptoms in some patients while others seem to still retain resistance to treatment, likely resulting from the contribution of other IL-17 isoforms (e.g. IL-17F), TNFα, IL-22.
IMMUNE 3D® presents a unique system to cost effectively elucidate the role for T cells and other immune cells such as macrophages and neutrophils in the pathogenesis of psoriasis.
Several immune regulatory pathways naturally evolved to promote tolerance to self-antigens and other foreign beneficial antigens we encounter such as commensal microbes, food, reproduction. However, the pressures of convergent evolution mean detrimental invaders such as tumors or pathogenic microbes have learned how to co-opt these pathways to evade immunity and establish persistence. For example, activation of self-antigen specific T cells that escape deletion during thymic development is regulated by active suppression by immune suppressive regulatory T cells (Tregs) and engagement of cell-surface inhibitory receptors such as programmed cell death protein 1 (PD-1).
These studies, in addition to many others provides supporting evidence to begin broadening the focus of vaccination strategies beyond targeting humoral immunity to also promote expansion and retention of memory T cells. To generate these recombinant vaccines however requires identification of antigenic targets to promote an optimal T cell response with the breadth to recognize and clear potentially rapidly mutating pathogens.
While, in vivo murine and non-human primate models are important for testing vaccine efficacy in vivo, 3D culture with human target cells represents an important model for testing these vaccine strategies to determine optimal antigen selection and understand how immune cells within these tissues will respond to infection with or without vaccination. Furthermore, improved vaccination strategies can be developed through a better understanding of additional factors that may be present within the infected tissue (e.g. metabolism, cell-surface inhibitory receptors).
Fibrosis is characterized by excessive deposition of collagen and other extracellular matrix components in a variety of different organs. This typically results from hyperactivity of fibroblasts within or myofibroblasts within a given tissue. While fibrosis contributes to many different diseases (e.g. non-alcoholic steatohepatitis (NASH), pulmonary fibrosis, psoriasis, scleroderma) it likely is a result of disrupted regulation of a normal repair process in response to exogenous insults (e.g. physical trauma, infection). While in some capacity this could reflect intrinsic defects in these tissue cells (keratinocytes, fibroblasts) it is also likely exacerbated by increased and unperturbed inflammation within the tissue environment. Th1 predominant response is protective while imbalance of Th2 and Th17 cells leads to a pro-fibrotic milieu. However, the direct role of IL-17 in promoting or dampening fibrosis is controversial considering its expression is decreased in certain fibrotic disease patients.
IMMUNE 3D® aims to elucidate the role of lymphocyte migration and infiltration in regulating the fibrotic diseases.
Solid organ transplantation is the only curative treatment option for many patients with end stage disease; however, transplant recipients receive immunosuppressive therapies in order to block alloimmunity and prevent graft rejection. Unfortunately, these immunosuppressive agents can make transplant recipients more susceptible to infections and post-transplant malignancies. Thus, preclinical models are critical to develop a better understanding of posttransplant complications in order to alleviate the pathophysiological processes that lead to these issues, identify novel immunosuppressants, and develop innovative treatment strategies.
- Immune 3D® can be used as an in vitro model to identify compounds that inhibit fibrosis by creating a mixed lymphocyte reaction and assessing relevant factors such as fibroblast proliferation and TGF-b production
- Determine the efficacy of compounds that enhance the function or expansion of impact of specific populations (Tregs)
- Investigate the effectiveness of novel immunosuppressants on T cell migration, proliferation and effector functions compared to cyclosporine, FK506, and rapamycin.
